Interventional Oncology
Interventional Radiologists are doctors who specialize in minimally invasive, targeted treatments performed using imaging for guidance.
The interventional radiologists at Lake Medical Imaging are board-certified, fellowship-trained, and have added qualifications in interventional techniques.
In the office or in the hospital, patients can expect to receive the same excellent care. Our interventional radiologists and their staff are dedicated to helping their patients win the battle against disease.
By combining their expertise in diagnostic radiology with advanced training in minimally invasive techniques using image guidance, interventional radiologists diagnose and treat a variety of conditions, including cancer and benign tumors. By utilizing innovative and diagnostic modalities to deliver treatment directly to the source of the problem, there is often no need for surgery. They can also provide intravenous long-term access for delivery of intravenous treatment by your oncologists or infectious disease physicians with Port and PICC lines
For more information, visit: Society of Interventional Radiology/Patient Center/Cancer
Tumor Ablation
Microwave (MV) or radiofrequency ablation (RFA), or simply tumor ablation, is a minimally invasive therapy to eliminate tumors in the liver, kidneys, lungs, or bones. A special needle electrode is placed in the tumor under imaging guidance, such as CT.
You will consult with one of our interventional radiologists in order to determine if you are a candidate for the minimally invasive procedure. The radiologist will instruct you on how to prepare for the procedure. You will be advised to stop taking certain blood thinners several days prior to your procedure and instructed to not eat or drink anything for several hours beforehand. Leave jewelry at home and wear loose, comfortable clothing.
You will receive an IV for conscious sedation and an antibiotic. After sterile prep and use of a local anesthetic under CT guidance, a microwave or radio frequency probe is placed into the tumor. The energy delivered through the probe will ablate the tumor. There is typically minimal or no associated discomfort during or after the procedure, which takes approximately one hour.
You will remain in a recovery room until you are completely awake and ready to return home. You should be able to resume your usual activities within a day or two. No driving is permitted for 24 hours due to the conscious sedation given during the procedure.

Mahrad Paymani, M.D.
Cryoablation
The technique is similar to the microwave or radiofrequency ablation but uses freezing temperatures to ablate the tumor. This technique requires longer procedure time to ablate the tumor and may require the placement of several needles into the tumor during the ablation.
Yttrium-90 Radioembolization
Radio-embolization is a minimally invasive procedure that combines embolization and radiation therapy to treat liver cancer. Y-90 radioembolization is a catheter-based therapy that delivers internal radiation to hepatic tumors in the form of microspheres. Targeted treatment is delivered directly to liver tumors, sparing nearby healthy tissue as much as possible and reducing some side effects. Tiny glass or resin beads filled with the radioactive isotope Yttrium-90 are placed inside the blood vessels that feed a tumor. This blocks the supply of blood to the cancer cells and delivers a high dose of radiation to the tumor. It can help extend the lives of patients with inoperable tumors and improve their quality of life.
Several days prior to the procedure, you will have an office consultation with your interventional radiologist to discuss the pros and cons of the procedure and have your blood tested to assess your coagulation status as well as liver and kidney function (MELD score).
Leave jewelry at home and wear loose, comfortable clothing the day of the procedure. Arrange for a designated driver to drive you home afterward, and plan to restrict your contact with children and adults for three to seven days.
A technologist will insert an IV line into a vein in your hand or arm to administer a sedative. You will be escorted to an angiography suite where you will be positioned on your back and connected to monitors that track your heart rate, blood pressure and oxygenation. The area of your body where the catheter is inserted will be sterilized and covered with a surgical drape. Your physician will numb the area with a local anesthetic. This may briefly burn or sting before the area numbs. A tiny incision is made at the site.
A catheter approximately the size of a pen tip is guided under fluoroscopy into the desired vessels in your liver. Ionizing radiation via millions of tiny glass beads is then delivered into the tumor.
A technologist will insert an IV line into a vein in your hand or arm to administer a sedative. You will be escorted to an angiography suite where you will be positioned on your back and connected to monitors that track your heart rate, blood pressure and oxygenation. The area of your body where the catheter is inserted will be sterilized and covered with a surgical drape. Your physician will numb the area with a local anesthetic. This may briefly burn or sting before the area numbs. A tiny incision is made at the site.
A catheter approximately the size of a pen tip is guided under fluoroscopy into the desired vessels in your liver. Ionizing radiation via millions of tiny glass beads is then delivered into the tumor.
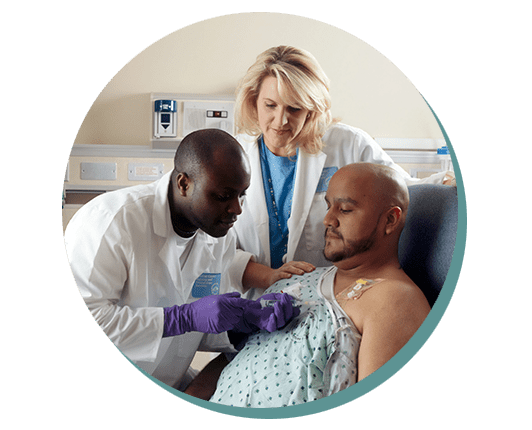
Image courtesy of National Cancer Institute. (Photographer: Rhoda Baer )
PORT Placement
Ports are often requested for chemotherapy or antibiotic infusions in order to prevent venous injury. They provide a relatively safe and easy access by the healthcare providers. After the initial healing process (when the port is not accessed), you can take showers or immerse the site in a pool of water without being concerned about infection. Ports can be kept even after the initial chemotherapy has been completed. The port needs to be flushed occasionally in order to maintain the patency of the port and its catheter. You can always request a consultation with your interventional radiologist before having a port placed.
You may be asked to stop taking certain blood thinners for a short time before and after the port placement, in order to prevent bleeding as a result of the procedure. Continue to take your other medications, if required. You may require a blood draw in order to assess your coagulation factors.
Leave jewelry at home on the day of your procedure. You will receive an IV access and be administered intravenous antibiotics, after which time you will be escorted into a fluoroscopy suite and sterile procedure room where you will be sedated. After sterile prep and use of local anesthetic, a 4 to 5 cm incision will be made on your upper left or right chest as well as a 1 cm incision for access into your jugular vein on the same side. The port will be placed under your skin and the catheter from the port will go into your jugular vein. Incisions will be closed and dressings placed on the incision sites. You will be able to go home one or two hours after the procedure. Arrange for a designated driver to drive you home, since you will receive conscious sedation during the procedure.
You may shower, but until the incisions are healed, no baths or immersion of the incision sites into a pool of water are allowed. You may remove the clear and gauze dressings after two days, but allow the white strips of paper tape (Steristrips) to fall off on their own. The port can be accessed immediately after placement. Do not immerse the port site in a pool of water while the port is accessed with a needle.
A catheter approximately the size of a pen tip is guided under fluoroscopy into the desired vessels in your liver. Ionizing radiation via millions of tiny glass beads is then delivered into the tumor.