Mammography and
Breast Imaging
When it comes to early detection of breast cancer, we have been leading the way for decades. In fact, we are #1 in breast cancer detection in the South U.S.*
From 3D screening mammography to breast MRI and the latest diagnostic technology, including Transpara AI, our full range of breast imaging provides customized care for all women. Because each woman is different, with differing breast density and history, we offer a full range of breast imaging solutions. We offer same-day results that eliminate potential weeks of worry, and, if anything unusual is detected, follow-up imaging can be scheduled immediately.
*According to the National Mammography Database
Screening Mammograms
Mammograms save lives. Screening mammograms allow radiologists to find abnormalities even before they can be felt during a physical exam. When detected early, breast cancer has a 95% cure rate.
The American College of Radiology (ACR) and the Society for Breast Imaging recommend an annual screening mammogram beginning at age 40, for women with an average risk of breast cancer. Women with a family history may need to start mammography sooner and/or include supplemental imaging in their screening plan.
National Cancer Network: Breast cancer risk assessments at 25, mammos at 40 for normal-risk women. Read More
Webinar Presented by Dr. Cathrine Keller – Lake Medical Imaging With Volpara and Ambry Genetics: Breast Screening
A Guide to Understanding Breast Biopsy Results
A breast biopsy may be ordered when a mammogram or another imaging test detects something out of the ordinary that would benefit from further exploration. Please keep in mind that while most biopsy results do not indicate the presence of cancer, a few will require follow-up treatment. The download below explains some of the terms that may be used in your biopsy results, to tell you what has been found in your breast.
Download the Society of Breast Imaging Guide to Breast Biopsy Results.
Dense Breast Tissue
Dense breast tissue is made up of glands and fibrous tissue and is an independent risk factor in and of itself for breast cancer. Fortunately, there are new technologies, such as contrast-enhanced mammography, breast MRI, and automated breast ultrasound (ABUS) that allow us to customize breast imaging according to the patient’s breast density so that cancer can be identified in its earliest, most treatable stage.
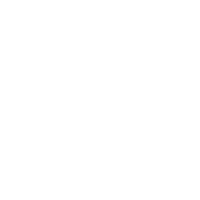
3D Mammography
Lake Medical Imaging offers state-of-the art 3D mammography in all of our offices. This test is recommended when it can help your physician obtain the images he or she needs to make a more confident diagnosis and determine the next steps in your care. It is often used with women who have more dense breast tissue, as it helps clinicians see behind normal breast tissue where abnormalities could hide and between overlapping breast tissues.
SenoClaire Digital Breast Tomosynthesis provides physicians with clear 3D breast images in multiple slices so that they can view breast tissue in layers, look between overlapping tissue, and identify abnormalities.
It is one component of our technologies and services designed to help detect disease earlier, provide more confident diagnoses and create personalized treatment plans…for every woman.
Diagnostic Mammograms
Used to evaluate a patient with abnormal symptoms such as a breast lump, nipple discharge or dense breast tissue that may have been noticed during an exam or screening mammogram.
Screening mammogram appointments do not require a physician’s referral and can be requested by calling 352-365-0777.
Planning for your mammogram
Tell your doctor about any breast symptoms or problems, prior surgeries, hormone use, whether you have a family or personal history of breast cancer, and if there's a possibility you are pregnant. You will be asked to obtain copies of your prior mammograms if at all possible. Leave jewelry at home and wear loose, comfortable clothing. Don't wear deodorant, talcum powder or lotion under your arms or on your breasts as these may appear on the mammogram and interfere with correct diagnosis.
What can I expect during this procedure?
You will feel pressure on your breast as it is squeezed by the compression paddle. Always remember compression allows the radiologist to view breast tissue more clearly for a better-quality mammogram.
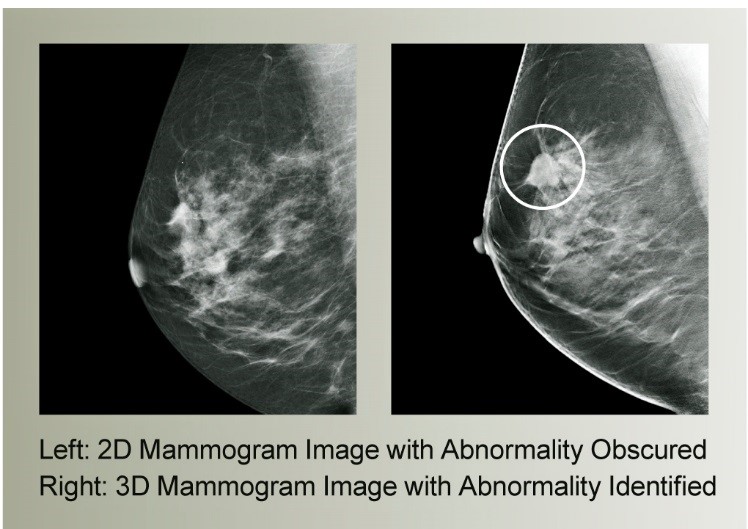
After a radiologist analyzes the images, preliminary results will be given to you during your visit with us. A full report will then be sent to your referring physician.
Follow-up exams may be needed. Sometimes a follow-up exam is done because the radiologist is unable to get the complete diagnostic picture that they need due to breast density or other factors. In some cases, a potential abnormality needs further evaluation with additional views or a special imaging technique. A follow-up exam may also be done to see if there has been any change in an abnormality over time. Follow-up exams are fairly routine and are not cause for alarm.
Breast Ultrasound
Ultrasound imaging of the breast uses sound waves to produce pictures of the internal structures of the breast. It is primarily used to help diagnose breast lumps or other abnormalities your doctor may have found during a physical exam, mammogram or breast MRI. Ultrasound is safe, non-invasive and does not use radiation.
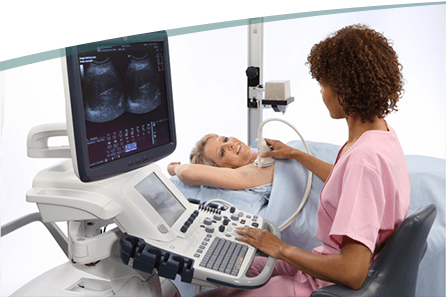

Automated Breast Ultrasound (ABUS)
Although ultrasound has shown it can increase breast cancer detection when added to mammography, traditional hand-held ultrasound is not always the best choice for imaging dense breast tissue. With 3D ultrasound volumes and ABUS software, radiologists can peruse hundreds of breast tissue image “slices,” looking at layers of dense tissue to find breast cancers that may have been missed on a mammogram.
ABUS exams use compression and take approximately 20 minutes. This procedure requires little to no special preparation. Leave jewelry at home and wear loose-fitting, comfortable clothing. You will be asked to undress from the waist up and to wear a gown during the procedure.
The ABUS system was created specifically for breast screening. It automates the imaging process to help provide remarkable image quality, consistency, reproducibility, and sensitivity of whole breast ultrasound in women with dense breasts. ABUS can help physicians provide answers sooner regarding the presence or absence of breast cancer.
Planning for your breast ultrasound
This procedure requires little to no special preparation. Leave jewelry at home and wear loose-fitting, comfortable clothing. You will be asked to undress from the waist up and to wear a gown during the procedure.
After being positioned on the exam table, a clear gel is applied in the area being examined; it may feel a bit cold. The gel helps the transducer make contact with the skin. The technologist firmly presses the transducer against the breast and moves it back and forth to image the area of interest.
After a radiologist analyzes the images, preliminary results will be given to you during your visit with us. A full report will then be sent to your referring physician.

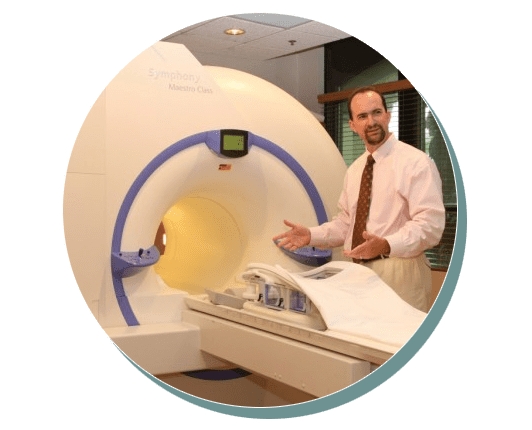
George E. Kainz, M.D. – Breast MRI is the most sensitive and thereby considered by most experts to be the best imaging technology available for detecting breast cancer.
Breast MRI
What is Breast MRI and how is it useful?
Based on the results of your last mammogram, or your medical/family history of breast cancer, your physician may recommend a breast MRI exam.
Breast MRI is the most sensitive, and thereby considered by most experts to be the best imaging technology available for detecting breast cancer. Since a breast MRI detects almost all invasive breast cancers, even the smallest, it is revolutionizing the way we diagnose and treat breast cancer.
Unlike mammography, breast MRI uses no radiation. Instead, radiofrequency waves in a magnetic field create hundreds of images of the breast. The images are captured digitally in three dimensions and show an incredible amount of fine detail. The use of an intravenous contrast called gadolinium is required to best detect breast cancers.
At Lake Medical Imaging, we utilize a special computer-assisted detection (CAD) program designed for the processing and interpretation of Breast MRI Images, in addition to the interpretation by our board-certified radiologists who specialize in breast imaging. These exams are performed at our MRI Centers in Leesburg and The Villages.
Planning for your breast MRI
No eyeglasses, jewelry, dentures, hearing aids, or metallic objects of any kind can be brought into the MRI exam room. You will be provided with a gown to wear during the imaging process.
A breast MRI exam is performed with the patient lying on her stomach with her breasts placed in two specially designed cushioned breast cups below her. Prior to the exam, a technologist will start an IV to administer gadolinium, a special contrast material used to enhance breast tissue. Earplugs or headphones are given to each patient to insure maximum relaxation during the 30- to 40-minute exam. The technologist will step into the control area, while staying in constant contact both visually and using the intercom.
A full report will be sent to your referring physician within 48 hours of your exam.
SenoBright Contrast Enhanced Mammography

The SenoBright exam is a simple, quick, five-to-ten-minute procedure that is similar to a regular mammography exam, but with the injection of a small amount of iodine contrast agent prior to the exam.
For a woman facing even the slightest hint of a breast cancer diagnosis, the answers can’t come soon enough. That’s why we have made SenoBright Contrast Enhanced Spectral Mammography (CESM) available to our patients soon after an abnormal mammogram. In addition, CESM helps to see through dense breast tissue to find breast cancers that are hiding on a mammogram, and it helps to resolve complex breast patterns not resolved with extra mammography views and/or breast ultrasound. Performed as an adjunct to an inconclusive mammogram or ultrasound exam, SenoBright highlights areas of unusual blood flow patterns that may be cause for increased suspicion of the presence of cancer. CESM is one of the most powerful diagnostic tools to help physicians diagnose the presence or absence of breast cancer.
Please note that our Senobright exam is classified as a diagnostic mammogram. When this exam is performed, coverage may vary based on your insurance plan. As a result, the service may be applied toward your deductible, copayment, or coinsurance, and you may have an out-of-pocket responsibility. We recommend verifying your benefits with your insurance provider for specific coverage details.
For more information, watch the short video about: SenoBright Contrast Enhanced Spectral Mammography
Download this brochure to learn more about your upcoming SenoBright Exam
For more information, read: SenoBright Mammography Gave My Doctors the Information They Needed
Serena Bright Contrast-Guided Breast Biopsy
It works in combination with SenoBright to help our radiologists see potentially cancerous areas more clearly, and to precisely target and guide where the anesthesia and biopsy needles are placed.
Learn more about FDA-approved Serena Bright and how it works in conjunction with SenoBright
Watch this short video about what you can expect during a
breast biopsy performed with Serena Bright.